Gastrointestinal Tract 3 (15-1 - )
General
15-1 (117A3) Which of the following may be observed after a total gastrectomy? Choose three.
a) Gallstones
b) Obesity
c) Anemia
d) Impaired glucose tolerance
e) Portal hypertension
The correct answers are:
a) Gallstones
c) Anemia
d) Impaired glucose tolerance
Explanation:
After a total gastrectomy, patients can experience several complications or changes due to the alteration in the digestive tract and the body's ability to process and absorb nutrients. The three conditions that may commonly occur are:
- The removal of the stomach can affect the regulation of bile flow, increasing the risk of gallstone formation. Changes in gut hormones and altered bile acid circulation after gastrectomy can promote the formation of gallstones.
- Anemia is a common post-gastrectomy complication due to decreased absorption of iron, vitamin B12, and folate. The stomach plays a critical role in the absorption of vitamin B12 and iron, and its removal can lead to deficiencies causing anemia.
- After gastrectomy, the rapid passage of food into the small intestine (dumping syndrome) can lead to fluctuations in blood sugar levels, resulting in impaired glucose tolerance or even postprandial hyperglycemia and hypoglycemia.
15-2 (117A14) Which symptoms of gastroesophageal reflux disease (GERD) are less likely to occur?
a) Chest pain
b) Diarrhea
c) Acid regurgitation
d) Sore throat
e) Chronic cough
The symptom less likely to occur in gastroesophageal reflux disease (GERD) is:
b) Diarrhea
Explanation:
GERD primarily affects the esophagus and is characterized by symptoms such as acid regurgitation (c), chest pain (a), sore throat (d), and chronic cough (e) due to the backward flow of stomach contents into the esophagus. Diarrhea is not a typical symptom of GERD as it mainly involves the upper gastrointestinal tract, specifically the esophagus, rather than affecting the digestive process or bowel movements directly.
15-3 (117C11) Which organs are fixed in the retroperitoneum?
a) Esophagus
b) Stomach
c) Duodenum
d) Jejunum
e) Transverse colon
The correct answer is:
c) Duodenum
Explanation:
The duodenum is part of the small intestine that is largely fixed in the retroperitoneum. This means it is located behind the peritoneum, the lining of the abdominal cavity, making it one of the structures that do not move freely within the abdominal cavity. The esophagus (a), stomach (b), jejunum (d), and transverse colon (e), in contrast, are not primarily retroperitoneal organs. The esophagus is a mediastinal structure before it enters the stomach, the stomach and jejunum are intraperitoneal and have mesenteries allowing for movement, and the transverse colon, while having portions that are secondarily retroperitoneal, is primarily considered intraperitoneal due to its mesocolon.
15-4 (117F12) Which of them is useful for diagnosis by the presence of oral aphthae?
a) Intestinal tuberculosis
b) Crohn's disease
c) Diverticulosis of the colon
d) Ischemic colitis
e) Irritable bowel syndrome
The most likely answer is:
b) Crohn's disease
Explanation:
Crohn's disease is a type of inflammatory bowel disease (IBD) that can affect any part of the gastrointestinal tract, from the mouth to the anus, though it most commonly affects the end of the small intestine (ileum) and the beginning of the colon. One of the extraintestinal manifestations of Crohn's disease is the presence of oral aphthous ulcers or aphthae. These are painful, shallow ulcers that can occur in the mouth and are thought to reflect the systemic nature of the disease. While oral aphthae can occur in various conditions, their presence in someone with gastrointestinal symptoms may suggest Crohn's disease, especially when other symptoms consistent with IBD are present.
Clinical
16-1 (117A20) A 62-year-old man visited the hospital with epigastric pain and dysphagia. He had been experiencing epigastric pain for six months but had postponed seeking medical attention due to work commitments. The pain persisted, and two weeks ago, when anorexia developed, he consulted a doctor. His medical history is unremarkable, and he has no history of smoking. He has been drinking a glass of soju daily for 40 years. His father had gastric cancer and underwent surgery at age 70. The patient's current measurements are a height of 170 cm and a weight of 52 kg, having lost 8 kg over the past six months. His body temperature is 36.8°C, pulse 80/min, blood pressure 128/72 mmHg. Mild anemia is noted in the eyelid conjunctiva without jaundice in the ocular conjunctiva. A palpable lymph node, 2 cm in diameter, is present in the left supraclavicular fossa. A mass, 5 cm in diameter, is palpable in the upper abdomen along with tenderness, but no abnormalities in intestinal sounds. Induration is palpated in the rectovesical pouch on digital rectal examination. Urinalysis shows protein (-), glucose (-), and ketones (+1). Blood tests reveal erythrocytes 3.68 million, Hb 8.9 g/dL, Ht 32%, leukocytes 9,300, platelets 210,000. Biochemical findings include total protein 6.5 g/dL, albumin 3.1 g/dL, total bilirubin 1.9 mg/dL, direct bilirubin 1.2 mg/dL, AST 128 U/L, ALT 116 U/L, LDH 277 U/L (standard 120-245), ALP 283 U/L (standard 38-113), γ-GT 132 U/L (standard 8-50), urea nitrogen 12 mg/dL, creatinine 1.6 mg/dL, glucose 98 mg/dL, CEA 38 ng/mL (standard ≤ 5), CA19-9 98 U/mL (standard ≤ 37), CRP 3.0 mg/dL. Upper gastrointestinal endoscopy diagnosed advanced gastric cancer. Contrast CT scans of the cervical, thoracoabdominal, and pelvic regions revealed multiple liver metastases, lymph node metastases, and peritoneal dissemination.
Which of these responses is inappropriate?
a) Schedule a total gastrectomy.
b) Discuss again in the presence of the family.
c) Inquire why surgery is desired.
d) Confirm the patient's understanding of their medical condition.
e) Explain the option of seeking a second opinion.
The inappropriate response for this patient, who has advanced gastric cancer with multiple liver metastases, lymph node metastases, and peritoneal dissemination, is:
a) Schedule a total gastrectomy.
Explanation:
Scheduling a total gastrectomy for a patient with extensive metastatic disease is generally not considered appropriate due to the advanced stage of the cancer. Surgery at this stage is unlikely to offer curative benefits and may not significantly extend life expectancy or improve quality of life. The focus for such advanced cases typically shifts towards palliative care to manage symptoms and maintain the quality of life, rather than aggressive surgical interventions. In this context, discussing the situation further with the family (b), inquiring about the patient's wishes regarding surgery (c), ensuring the patient understands their medical condition (d), and explaining the option of seeking a second opinion (e) are all appropriate steps. Scheduling a major surgery like a total gastrectomy without considering the advanced nature of the disease and the patient's overall condition and wishes would not be the right approach.
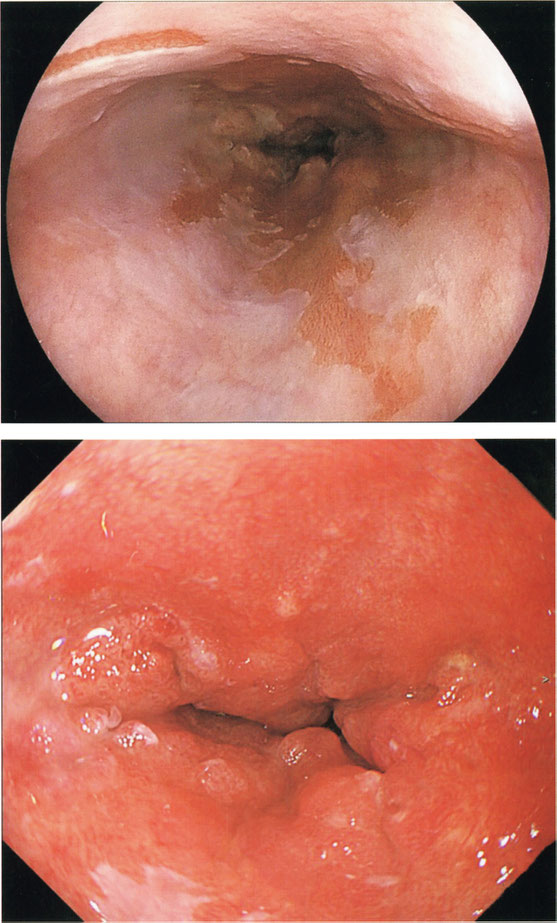
16-2 (117A36) A 60-year-old man visited the hospital due to lower abdominal pain. He had been experiencing a low-grade fever and lower abdominal pain for three days, which gradually worsened. Despite feeling nauseous and losing his appetite, he hasn't vomited. The pain in his lower abdomen persists and isn't alleviated by bowel movements, and he reports neither diarrhea nor constipation. At 22, he had his appendix removed. He isn't on any medications and has no history of smoking. He drinks a cup of Japanese sake nightly and has no notable family medical history. A year ago, during a medical check-up, a lower gastrointestinal endoscopy indicated diverticulosis in the large intestine. Currently, he is 175 cm tall and weighs 70 kg, with a temperature of 37.1°C, a pulse of 96/min, blood pressure of 136/88 mmHg, and a respiratory rate of 14/min. His SpO2 is 98% on room air. There are no abnormalities noted in his conjunctiva. The lower abdomen appears flat in the midline, with no signs of muscular defense or rebound pain, and neither the liver nor spleen is palpable. Intestinal sounds are normal, and urinalysis shows no protein, sugar, or occult blood. Blood tests reveal 4.68 million red blood cells, hemoglobin of 13.9 g/dL, hematocrit of 42%, and 12,300 leukocytes (with 30% band neutrophils and 45% segmented neutrophils), along with 200,000 platelets. Biochemical tests show a total protein of 7.5 g/dL, albumin of 3.9 g/dL, total bilirubin of 0.9 mg/dL, AST of 28 U/L, ALT of 16 U/L, LDH of 177 U/L (within the standard range of 120-245), ALP of 83 U/L (standard 38-113), gamma-GT of 48 U/L (standard 8-50), and amylase of 95 U/L (standard 37-160), with urea nitrogen at 12 mg/dL, creatinine at 0.6 mg/dL, glucose at 98 mg/dL, and CRP at 3.2 mg/dL. Images from last year's sigmoid colon endoscopy and the current visit's abdominal contrast CT are provided.
What is the appropriate course of action for this patient?
a) Enema
b) Colectomy
c) Administration of antimicrobials
d) Extracorporeal shock wave lithotripsy
e) Administration of corticosteroids


Given the patient's history, clinical presentation, and imaging findings, the appropriate response to this patient is:
c) Antimicrobial administration
Explanation:
The patient's symptoms of low-grade fever, lower abdominal pain, and a history of diverticulum of the large intestine, combined with an elevated white blood cell count (indicating an inflammatory response), suggest an episode of diverticulitis. Diverticulitis often presents with lower abdominal pain, fever, and changes in bowel habits, which align with this patient's symptoms. The absence of vomiting and the normal results of urinary findings further support this diagnosis. Additionally, the presence of diverticulum noted in a previous lower gastrointestinal endoscopy corroborates this assessment.
Treatment for uncomplicated diverticulitis typically involves antibiotics to target the infection and inflammation, making antimicrobial administration the most suitable approach. This is aimed at treating the underlying infection and preventing complications. An enema (a), colectomy (b), extracorporeal shock wave lithotripsy (d), and corticosteroid administration (e) are not indicated based on the information provided and the suspected diagnosis of uncomplicated diverticulitis. Corticosteroids, for example, would be contraindicated due to their immunosuppressive effects, which could worsen an infectious process.
16-3 (117A42) Just edit English: A 60-year-old woman came to the hospital with a complaint of blood in her stool. She had been experiencing abdominal pain and watery diarrhea six times a day for a week and was receiving medication from a medical institution near her home. Her abdominal pain worsened and she started having bloody stools since yesterday, prompting her visit to the doctor. She has no cough or sputum. Her medical history is unremarkable, with no history of overseas travel. Her height is 146 cm, and she weighs 38 kg. Her body temperature is 37.6°C, pulse rate is 96/min, and blood pressure is 124/74 mmHg. Heart and breathing sounds are normal. The abdomen is flat, with tenderness observed in the left lower abdomen. The liver and spleen are not palpable. Intestinal peristalsis is enhanced. Blood tests show erythrocytes at 3.93 million, hemoglobin at 11.2 g/dL, hematocrit at 33%, leukocytes at 15,300, and platelets at 490,000. Biochemical findings include total protein at 6.6 g/dL, albumin at 3.2 g/dL, AST at 13 U/L, ALT at 11 U/L, LD at 138 U/L (standard 120 to 245), ALP at 72 U/L (standard 38 to 113), γ-GT at 10 U/L (standard 8 to 50), amylase at 40 U/L (standard 37 to 160), CK at 48 U/L (standard 30 to 140), urea nitrogen at 7 mg/dL, creatinine at 0.6 mg/dL, uric acid at 3.2 mg/dL, blood glucose at 103 mg/dL, sodium at 135 mEq/L, potassium at 3.7 mEq/L, and chloride at 99 mEq/L. CRP is 9.4 mg/dL. No abnormalities were observed on chest radiographs. Which diseases are possible?
a) Intestinal tuberculosis
b) Crohn's disease
c) Ischemic enteritis
d) Ulcerative colitis
e) Intestinal Behçet's disease

The correct answer is:
d) Ulcerative colitis
Explanation:
The presence of bloody stools, abdominal pain, and watery diarrhea are hallmark symptoms of ulcerative colitis, a type of inflammatory bowel disease (IBD) that predominantly affects the colon and rectum. The enhanced intestinal peristalsis and tenderness in the left lower abdomen could indicate inflammation in the sigmoid colon, which is commonly affected by ulcerative colitis. The elevated CRP level supports the presence of an inflammatory process, and the absence of a history of overseas travel reduces the likelihood of intestinal tuberculosis (a). Although Crohn's disease (b), another type of IBD, could present with similar symptoms, it usually affects any part of the gastrointestinal tract and might present with more systemic symptoms. Ischemic enteritis (c) and intestinal Behçet's disease (e) are less common and have distinct clinical features not entirely aligned with this patient's presentation. Ulcerative colitis' characteristic feature of continuous colonic involvement starting from the rectum, leading to bloody diarrhea and abdominal pain, aligns with the symptoms described.
16-4 (117A51) A 76-year-old woman came to the hospital complaining of nausea and vomiting. She had been experiencing nausea for 3 months. Subsequently, vomiting began, and she started to vomit even without consuming food, prompting her to seek medical attention. Her medical history is unremarkable, with no history of smoking or drinking. She stands 150 cm tall and weighs 37 kg. Her pulse rate is 68/min, blood pressure 110/60 mmHg, and respiratory rate 14/min. Blood tests reveal erythrocytes at 3.92 million, Hb 10.9 g/dL, Ht 36%, leukocytes 4,100, and platelets 220,000. Blood biochemical findings include total protein 5.8 g/dL, albumin 3.2 g/dL, total bilirubin 0.5 mg/dL, AST 22 U/L, ALT 8 U/L, γ-GT 11 U/L (standard 8 to 50), urea nitrogen 22 mg/dL, creatinine 0.8 mg/dL, Na 131 mEq/L, K 3.4 mEq/L, Cl 96 mEq/L, CEA 16.4 ng/mL (standard 5 or less), and CA19-9 180 U/mL (standard 37 or less).
What is the appropriate method of nutrition until surgery?
a) Peripheral venous nutrition
b) Oral intake of dietary supplements
c) Enteral feeding with a nasogastric tube
d) Intravenous administration of albumin preparations
e) High-calorie infusion via central venous nutrition

The correct answer is:
e) High-calorie infusion via central venous nutrition
Explanation:
Her nutritional needs are significant, and her ability to tolerate enteral feeding might be compromised, possibly due to the severity of her symptoms or the risk of further nausea and vomiting. Central venous nutrition (also known as parenteral nutrition) allows for the delivery of a higher calorie content directly into the bloodstream, bypassing the gastrointestinal tract entirely. This method is beneficial for patients who cannot meet their nutritional needs through oral or enteral routes due to issues like severe gastrointestinal dysfunction, obstruction, or in cases where enteral nutrition might exacerbate symptoms. It's crucial, however, to monitor for potential complications associated with central venous nutrition, such as infections or liver dysfunction, especially in elderly patients.
16-5 (117A54) A 33-year-old man was brought in by ambulance due to severe pain in his lower right abdomen. He had experienced discomfort in his lower abdomen since yesterday, and as the pain gradually intensified to an unbearable level, he called for an ambulance. He has a history of an appendectomy performed at the age of 24. His oxygen saturation is 97% on room air. There are no abnormalities observed in the palpebral or ocular conjunctiva, heart sounds, or breathing sounds. The abdomen is flat, with positive Blumberg's sign and muscular defense noted in the right lower abdomen. Intestinal sounds are diminished. Blood tests show erythrocytes at 4.86 million, hemoglobin at 15.0 g/dL, hematocrit at 44%, leukocytes at 18,000 (with 82% neutrophils, 1% eosinophils, 1% basophils, 6% monocytes, and 10% lymphocytes), and platelets at 260,000. PT-INR is 0.9 (within the standard range of 0.9 to 1.1). Biochemical tests reveal total protein at 8.1 g/dL, albumin at 5.1 g/dL, total bilirubin at 1.2 mg/dL, AST at 23 U/L, ALT at 30 U/L, LD at 166 U/L (within the standard range of 120 to 245), ALP at 39 U/L (within the standard range of 38 to 113), γ-GT at 25 U/L (within the standard range of 8 to 50), amylase at 44 U/L (within the standard range of 37 to 160), CK at 64 U/L (within the standard range of 30 to 140), urea nitrogen at 17 mg/dL, creatinine at 1.2 mg/dL, uric acid at 6.4 mg/dL, blood glucose at 109 mg/dL, sodium at 140 mEq/L, potassium at 3.9 mEq/L, chloride at 101 mEq/L, calcium at 9.8 mg/dL, and CRP at 19 mg/dL. An abdominal contrast-enhanced CT scan is shown below.
Which treatment is appropriate for this patient?
a) Emergency surgery
b) High-pressure enema
c) Laxatives
d) Ileus tube placement
e) Laparocentesis drainage

The correct answer is:
a) Emergency surgery
Explanation:
Given the severity of the symptoms described—severe lower right abdominal pain, positive Blumberg's sign, muscular defense, elevated CRP, history of appendectomy, and the patient's presentation via ambulance indicating an emergency condition—the most appropriate course of action needs to be identified with urgency.
- Emergency surgery is the most fitting option given the critical symptoms, suggesting a potentially life-threatening condition such as an abscess, perforation, or another complication. This option allows for direct investigation and resolution of the issue.
- High-pressure enema (b), laxatives (c), and ileus tube placement (d) are generally not suitable for acute severe conditions indicated by these clinical signs. These methods are more commonly associated with managing bowel obstruction or constipation, which do not align with the acute presentation and likely diagnosis in this scenario.
- Laparocentesis drainage (e) might be considered for fluid accumulation or diagnostic purposes but does not address the immediate need suggested by acute severe pain and inflammatory markers.
16-6 (117A56) A 26-year-old man came to the hospital with abdominal pain. He has experienced abdominal pain and diarrhea for the past 6 years. Since starting his job, his symptoms have worsened, leading to frequent tardiness and absences from work. Other symptoms include heartburn after overeating for the past six months. His body temperature is 36.0°C, pulse 96/min, and blood pressure 120/60 mmHg. There is no anemia observed in the eyelid conjunctiva, and no abnormalities in heart and lung sounds. The abdomen is flat with mild tenderness in the lower abdomen; the liver and spleen are not palpable. Intestinal peristalsis is mildly enhanced. Blood findings show erythrocytes 5.05 million, Hb 15.0 g/dL, Ht 45%, leukocytes 7,300, and platelets 260,000. Blood biochemical findings indicate total protein 7.9 g/dL, albumin 5.0 g/dL, AST 17 U/L, ALT 13 U/L, LD 130 U/L (standard 120 to 245), ALP 73 U/L (standard 38 to 113), γ-GT 15 U/L (standard 8 to 50), Amylase 60 U/L (standard 37 to 160), CK 61 U/L (standard 30 to 140), Urea nitrogen 12 mg/dL, Creatinine 0.6 mg/dL, Uric acid 4.8 mg/dL, Blood glucose 98 mg/dL, Na 140 mEq/L, K 3.9 mEq/L, Cl 102 mEq/L, CRP 0.1 mg/dL. A fecal occult blood test was positive. A lower gastrointestinal endoscopy was performed to investigate the cause.
Which of the underlined areas is the basis for performing lower gastrointestinal endoscopy in this patient?
a) Heartburn
b) Body temperature
c) Pulse and blood pressure
d) Blood findings
e) Positive fecal occult blood test
The correct answer is:
e) Positive fecal occult blood test
Explanation:
Given the context, the most relevant information prompting lower gastrointestinal endoscopy in this patient is the presence of a positive fecal occult blood test, which is indicated by Positive fecal occult blood test. This finding suggests the possibility of hidden bleeding within the gastrointestinal tract, which could be due to various conditions, including polyps, cancers, inflammatory bowel diseases, or other sources of bleeding that necessitate direct visualization and possibly biopsy for diagnosis.
16-7 (117A58) A 72-year-old man came to the hospital with a complaint of heartburn. He had been experiencing heartburn after eating since the age of 60, but he managed his symptoms by reducing his diet. However, symptoms resumed two weeks ago, prompting him to seek medical attention. He has no history of smoking or drinking. His consciousness was clear, height 170 cm, weight 78 kg, BMI 27.0, body temperature 36.6°C, pulse rate 80/min, blood pressure 128/84 mmHg, respiratory rate 15/min, and SpO2 96% (room air). There was no anemia in the palpebral conjunctiva or yellowing in the ocular conjunctiva. Urine findings: protein (-), sugar (-), occult blood (-). Blood findings: red blood cells 4.8 million, Hb 13.9 g/dL, Ht 46%, leukocytes 5,200, platelets 250,000. Blood biochemical findings: total protein 6.6 g/dL, albumin 3.9 g/dL, total bilirubin 0.9 mg/dL, AST 20 U/L, ALT 28 U/L, LD 170 U/L (standard 120-245), ALP 110 U/L (standard 38-113), γ-GT 45 U/L (standard 8-50), amylase 90 U/L (standard 37-160), urea nitrogen 12 mg/dL, creatinine 0.8 mg/dL, blood glucose 98 mg/dL, CRP 0.5 mg/dL. An upper gastrointestinal endoscopy revealed an image of the lower esophagus, and adenocarcinoma was diagnosed through a pathological examination of the endoscopic biopsy.
Which of the following is possible in the pathology of this patient? Choose three.
a) Continuous cylindrical epithelium from the stomach is found in the esophagus.
b) The lower esophageal sphincter is less relaxed.
c) Stomach acid tends to flow back into the esophagus.
d) It is considered a hereditary disease.
e) Obesity is involved.
The pathology of the patient described suggests Barrett's esophagus, which is a condition that can lead to esophageal adenocarcinoma. The correct answers, based on the provided information, are:
a) Continuous cylindrical epithelium from the stomach is found in the esophagus.
c) Stomach acid tends to flow back into the esophagus.
e) Obesity is involved.
Explanation:
- Continuous cylindrical epithelium from the stomach is found in the esophagus. This describes the condition known as Barrett's esophagus, where the normal squamous epithelium of the esophagus is replaced with columnar epithelium similar to that of the stomach or intestine, usually due to chronic gastroesophageal reflux disease (GERD).
- Stomach acid tends to flow back into the esophagus. This indicates GERD, which is a major risk factor for the development of Barrett's esophagus and subsequent esophageal adenocarcinoma.
- Obesity is involved. Obesity, particularly central obesity, is a known risk factor for GERD and, by extension, Barrett's esophagus and esophageal adenocarcinoma due to increased intra-abdominal pressure causing reflux.
- Options b and d are less relevant to the pathology indicated by the patient's symptoms and diagnosis. The relaxation of the lower esophageal sphincter is indeed involved in GERD, but it is not directly implicated in the patient's pathology regarding the development of adenocarcinoma (b). While there may be genetic components to Barrett's esophagus and esophageal adenocarcinoma, it's not predominantly considered a hereditary disease (d), making it a less likely choice for this context.
16-8 (117A62) A 40-year-old man presented to the hospital with complaints of heartburn, which started two months ago as a sensation of tightness while eating and evolved into heartburn two weeks prior. He has a long-standing history of atopic dermatitis, treated since he was 16, but does not smoke. He has consumed beer daily (350 mL/day) for the past 20 years. His family medical history is unremarkable. Upon examination, he is alert with a height of 172 cm and weight of 60 kg. His body temperature is 36.2°C, pulse rate is 76/min, blood pressure is 126/78 mmHg, and respiratory rate is 14/min with an SpO2 of 99% on room air. The skin shows erythema, papules, and crusts symmetrically on the face, neck, trunk, and extremities. There are no abnormalities noted in the eyelid or ocular conjunctiva, no goiter or palpable cervical lymph nodes, and the abdomen is flat, soft, and non-tender. Laboratory findings indicate erythrocytes at 4,580,000, Hb 13.7 g/dL, Ht 41%, leukocytes at 7,300 (with a distribution including 20% rod-shaped neutrophils, 30% lobular nucleus neutrophils, 8% eosinophils, 1% basophils, 6% monocytes, and 35% lymphocytes), and platelets at 240,000. Biochemical analysis shows total protein at 7.9 g/dL, albumin at 4.2 g/dL, total bilirubin at 0.9 mg/dL, AST at 24 U/L, ALT at 18 U/L, LD at 178 U/L, ALP at 86 U/L, γ-GT at 38 U/L, amylase at 85 U/L, urea nitrogen at 20 mg/dL, creatinine at 0.8 mg/dL, blood glucose at 92 mg/dL, and CRP at 0.1 mg/dL. Despite being prescribed proton pump inhibitors, his symptoms have not improved.
What potential conditions could this patient be experiencing?
a) Esophageal cancer
b) Gastroesophageal Reflux Disease (GERD)
c) Eosinophilic esophagitis
d) Esophageal achalasia
e) Esophageal candidiasis


The correct answer is:
c) Eosinophilic esophagitis
Explanation:
Given the patient's long-standing history of atopic dermatitis, a known association with eosinophilic esophagitis (EoE), and the lack of symptom improvement with proton pump inhibitors, Eosinophilic esophagitis is a highly probable diagnosis. EoE is an immune/antigen-mediated esophageal disorder characterized by eosinophilic infiltration of the esophageal epithelium, which is commonly associated with allergic diseases, including atopic dermatitis. The symptoms of EoE, such as heartburn, dysphagia, and food impaction, can mimic those of GERD but do not typically respond well to proton pump inhibitors, which further supports the likelihood of EoE in this patient. The presence of eosinophilia in the blood could also hint towards an allergic or eosinophilic condition, aligning with the diagnosis of eosinophilic esophagitis.
16-9 (117A65) A 56-year-old woman visited the hospital due to persistent discomfort in her epigastric region that she had been experiencing for half a year. Her medical history is unremarkable. She stands at 162 cm and weighs 61 kg. Examination shows no anemia in the eyelid conjunctiva and no abnormalities in heart and lung sounds. Her abdomen is flat and soft, with no palpable liver or spleen enlargement. Laboratory tests reveal erythrocytes count at 3.99 million, hemoglobin at 11.5 g/dL, hematocrit at 35%, leukocytes at 4,300, and platelets at 170,000. Biochemical tests show total protein at 7.2 g/dL, albumin at 4.1 g/dL, total bilirubin at 0.5 mg/dL, AST at 20 U/L, ALT at 16 U/L, LD at 184 U/L (standard 120-245), urea nitrogen at 21 mg/dL, creatinine at 0.9 mg/dL, blood glucose at 93 mg/dL, and CRP at 0.2 mg/dL. The upper gastrointestinal endoscopy image (A) and biopsy histology (H-E staining, KIT immunostaining, αSMA [smooth muscle actin] immunostaining) (B) are presented below. Which is the most suitable treatment?
a) Follow-up
b) Radiation therapy
c) Partial gastrectomy
d) Treatment with cytotoxic drugs
e) Treatment with endocrine (hormonal) drugs


The correct answer is:
c) Partial gastrectomy
Explanation:
Given the information provided and the inclusion of biopsy histology with specific immunostaining, it suggests the presence of a lesion that was investigated further through endoscopic biopsy. The choice of immunostaining techniques like KIT and αSMA indicates a diagnostic approach towards gastrointestinal stromal tumors (GISTs) or other mesenchymal tumors, where KIT immunostaining is particularly used to identify GISTs, and αSMA is used to identify smooth muscle actin in tumors.
The appropriate response in the case of a confirmed GIST, depending on its size, location, and risk assessment based on mitotic count and tumor size, could range from surgical resection to targeted therapy with tyrosine kinase inhibitors (e.g., imatinib) if the tumor is unresectable, has metastasized, or as an adjuvant treatment post-surgery to reduce the risk of recurrence.
Given this context and without specific details on the tumor's characteristics from the biopsy results (e.g., size, mitotic index), the most generalized and likely appropriate response could be:
- Partial gastrectomy for a localized GIST with the potential for complete resection to achieve cure.
- Treatment with cytocidal drugs (d) might refer to the use of tyrosine kinase inhibitors like imatinib for GISTs that are positive for the KIT protein, although it is not the first choice here.
16-10 (117A74) An 88-year-old woman was brought to the hospital by ambulance due to melena. She noticed a painful bulge in her right lower abdomen in the morning and called for an ambulance upon noticing blood in her stool. Her blood pressure was 56 mmHg. The abdomen was distended with elevated intestinal sounds. A 3 cm diameter bulge was observed in the right groin area, which was tight and tender to the touch. Blood tests revealed: erythrocytes 3.68 million, Hb 12.9 g/dL, Ht 36%, leukocytes 15,600, platelets 210,000. Biochemical tests showed: total protein 6.5 g/dL, albumin 2.9 g/dL, total bilirubin 0.9 mg/dL, AST 28 U/L, ALT 26 U/L, LD 287 U/L (standard 120 to 245), CK 162 U/L (standard 30 to 140), urea nitrogen 44 mg/dL, creatinine 1.8 mg/dL, CRP 4.7 mg/dL.
Which of the following is the correct action?
a) Enema
b) Emergency surgery
c) Follow-up
d) Ileus tube placement
e) Puncture of the inguinal bulge

The correct action in this scenario is:
b) Emergency surgery
Explanation:
Given the patient's symptoms of melena (black, tarry stools indicative of gastrointestinal bleeding), a painful and tight bulge in the right lower abdomen (suggesting an incarcerated or strangulated hernia), and the urgent nature of her condition as evidenced by the call for an ambulance and the findings of elevated leukocytes (indicative of an infection or inflammation) and high CRP levels (another marker of inflammation or infection), emergency surgery is warranted. The presence of a bulge in the groin area likely represents a hernia, and the associated symptoms suggest it may be strangulated, a condition that can compromise blood flow to the entrapped bowel segment and lead to necrosis if not promptly addressed. The elevated urea nitrogen and creatinine levels further suggest renal strain, possibly due to dehydration or shock, common in acute abdominal emergencies. Emergency surgery is necessary to alleviate the hernia's incarceration or strangulation and to address any potential bowel ischemia or necrosis, thereby preventing further complications.
16-11 (117F53) An 11-year-old boy was brought to the hospital by his mother due to pain in the lower right abdomen. He experienced discomfort near the solar plexus in the morning but attended school. After eating lunch, he vomited, and his abdominal pain progressively worsened, prompting a visit to the hospital. His temperature was 38.5°C, pulse 108/min, blood pressure 118/62 mmHg, and respiratory rate 22/min. His oxygen saturation was 99% on room air. No abnormalities were observed in heart or lung sounds. Tenderness was localized to the lower right abdomen, with evident muscular defense. Blood tests showed red blood cells at 4.3 million, hemoglobin 12.6 g/dL, hematocrit 40%, leukocytes 13,500, and platelets 250,000. Blood biochemical results included total protein 6.8 g/dL, albumin 4.0 g/dL, AST 20 U/L, ALT 10 U/L, urea nitrogen 12 mg/dL, creatinine 0.5 mg/dL, sodium 140 mEq/L, potassium 4.0 mEq/L, chloride 102 mEq/L, and CRP 8.2 mg/dL.
Which physical finding is predicted in this patient?
a) Dance's sign
b) Murphy's sign
c) Rosenstein's sign
d) Courvoisier's sign
e) Grey-Turner's sign

The correct answer is:
c) Rosenstein's sign
Explanation:
The Rosenstein sign is a specific indicator of acute appendicitis, where pain is intensified when the patient lies on their left side as opposed to lying supine, especially during palpation of McBurney's point. This sign can help in the differential diagnosis of acute appendicitis by demonstrating that the pain is more pronounced in a position that further stretches the peritoneal lining over the inflamed appendix, hence increasing the patient's discomfort.
In the context of the patient's symptoms—fever, vomiting, localized pain in the right lower quadrant with muscular defense, and elevated CRP—a positive Rosenstein sign would further support the suspicion of acute appendicitis. This is because the sign specifically suggests irritation or inflammation in the appendix area, which aligns with the patient's clinical presentation and elevated white blood cell count, indicating an active infection or inflammation process likely related to appendicitis.